Has your doctor informed you that your recent mammogram indicates that you have dense breasts? If so, are you trying to determine if additional testing should be done to screen for breast cancer? If you're confused about what to do, you're not alone.
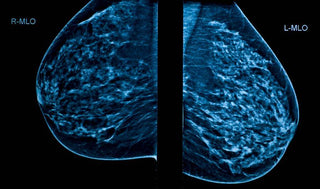
Breasts are made up of lobules and ducts along with fatty tissue and fibrous connective tissue. Breast density is a comparison of fatty tissue to fibrous connective tissue on a mammogram, so a dense breast has more connective tissue than fat.
Dense breasts are more frequent in younger women because as we grow older, our breasts become less dense. Mature women who use menopausal hormones may also have higher breast density until hormone treatment is stopped.
There are four categories of breast density ranging from almost entirely fatty to extremely dense. Breast density is not related to breast size or firmness but can be determined only by a mammogram.
Having dense breasts is linked to an increased risk of getting breast cancer as compared with women with less dense breasts.